Body Fluids and Circulation
INTRODUCTION : BODY FLUIDS AND CIRCULATION
We have learnt that all living cells have to be provided with nutrients, O2 and other essential substances. Also the waste or harmful substances produced, have to be removed continuously for healthy functioning of tissue. It is therefore, essential to have efficient mechanism for the movement of these substances to the cell and from the cell. Different group of animals have evolved different methods of transport.
HUMAN BLOOD
Blood is a mobile connective tissue composed of a fluid, the plasma and the cells, the blood corpuscles. Blood is the softest tissues in the body. Fluids outside the cells are generally called extracellular fluids (ECF). Blood forms about 30-35 percent of the ECF. The volume of blood in an adult person of 70 kg weight is about 5.5 litres. It is a slightly alkaline fluid having pH 7.4. pH of blood in arteries is more than in veins.
Composition
Blood consists of a watery fluid called plasma containing certain floating bodies termed formed elements. The latter include Red corpuscles, or Erythrocytes (RBCs) and White corpuscles or Leucocytes (WBCs) and Blood platelets or Thrombocytes.
The plasma and formed elements form about 55% and 45% of the volume of the blood respectively.
Plasma
The plasma is a faint yellow, slightly alkaline, viscous fluid.
| Sl. No. | Contents | % |
|---|---|---|
| 1. | Water | 90% |
| 2. | Proteins. (Albumen, Globulin, Prothrombin, Fibrinogen) | 7-8% |
| 3. | Inorganic Salts (Cations are Na, K, Mg, Ca, Fe and Mn, Anions are chloride, bicarbonate and phosphate) | 1% |
| 4. | Others (i) Food Materials (Glucose, Amino Acids, Fatty Acids, Triglycerides) (ii) Waste Materials (Urea, Uric, Acid and Creatine) (iii) Regulatory Substances (Hormone, Vitamins, Enzymes) (iv) Cholesterol (v) Antibodies (vii) Dissolved Gases (O2, CO2, N2) | 1-2% |
Red Blood Corpuscles (RBC’s)
The red blood corpuscles are the most numerous formed elements of the blood. They are the most abundant cells in the human body. A unique feature of the RBCs is the presence of a red, oxygen-carrying pigment, the haemoglobin, in their cytoplasm.
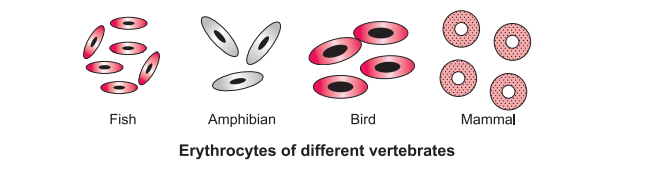
(a) Shape: The shape of RBCs varies in different vertebrate classes. In fishes, amphibians, reptiles and birds, they are oval, biconvex and nucleated. In mammals, they are circular, biconcave, enucleated discs. Camel and llama are exceptional among mammals in having oval RBCs.
Function- RBC contain haemoglobin, thus it helps in transporting gases to all the tissues. Each RBC contains approximately 280 million molecules of Hb. Oxygen is transported bound to Hb forming oxyhaemoglobin while CO2 bound to Hb forms carbamino Hb.
White Blood Corpuscles (WBC’s)
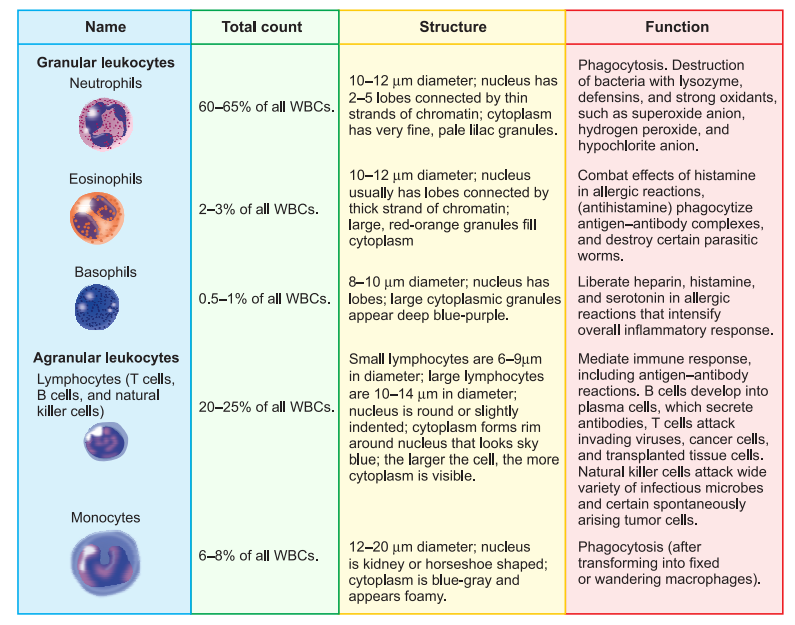
(a) Shape: The WBCs are rounded or irregular cells. They can change their shape and are capable of amoeboid movement. This enables them to squeeze out of capillaries into the tissues. This process is called diapedesis.
(b) Number: The WBCs are far fewer than the RBCs. Their number varies from 6,000 to 8,000 per cubic millimetre of blood. This number is the total count of WBC’s. It may increase or decrease abnormally in certain conditions. Rise in WBC count is called WBCs leucocytosis. It is a physiological response to infections (e.g., pneumonia), inflammations such as appendicitis, and malignancies such as leukemia (blood cancer). Fall in WBC count is termed leucocytopenia. It occurs in conditions such as folic acid deficiency, infection of AIDS virus. WBC count is useful in diagnosing diseases.
(c) Colour: The WBCs are colourless as they lack haemoglobin.
Platelets/Thrombocytes (a) Shape: The platelets are non-nucleated, rounded or oval, disc-like bodies.
(b) Size: The platelets are the smallest formed elements of the blood.
(c) Number: The platelets are fewer than the red corpuscles and more than the white corpuscles in number. There are about 1,50,000-3,50,000 platelets in a cubic millimetre of blood. Increase and decrease in the number of platelets is known as thrombocytosis and thrombocytopenia respectively.
(d) Function: It helps in blood clotting.
Haemopoiesis: The process of formation of blood is called haemopoiesis. The tissues in which blood is formed are termed haemopoietic tissues. These include red bone marrow and lymphoid tissues (spleen, thymus and lymphatic nodes).
Erythrocytes, leucocytes and platelets all arise from a common source, the pluripotent stem cells in the red bone marrow.
BLOOD GROUPS
- Blood groups are special characteristics of blood in humans and related primates due to the presence of genetically controlled antigens and antibodies.
- Two types of blood group are – ABO grouping & Rh grouping.
ABO Grouping
- ABO grouping (was the first to be discovered) is based on the presence or absence of two surface antigens (chemicals that can induce an immune response) on the RBCs namely A and B. Similarly, the plasma of different individuals contain two natural antibodies (proteins produced in response to antigens).
During blood transfusion, blood of donor must be matched with blood of recipient to avoid clumping or destruction of RBC’s.
- The distribution of antigens and antibodies in the four groups of blood, A, B, AB and O are:
| Blood Group | Antigens on RBCs | Antibodies in plasma (Serum) | Donor’s Group | Receivers Group |
|---|---|---|---|---|
| A | A | anti-B | A, O | A and AB |
| B | B | anti-A | B, O | B and AB |
| AB | A, B | nil | AB, A, B, O | AB |
| O | NIL | anti-A,B | O | O, A, B, AB |
- Group ‘O’ blood can be donated to persons with any other blood group and hence ‘O’ group individuals are called ‘universal donors’. Persons with ‘AB’ group can accept blood from persons with AB as well as the other groups of blood. Therefore, such persons are called ‘universal recipients’.
RH Grouping
- There are several other proteins in the blood that may bring about agglutination under certain conditions. The most important of these is Rh factor. The Rhesus (Rh) system was discovered by Landsteiner and Weiner in 1940.
- Antigen, the Rh antigen similar to one present in Rhesus monkeys (hence Rh) is observed on the surface of RBCs of majority (nearly 80 per cent) of humans. Such individuals are called Rh positive (Rh+ve) and those in whom this antigen is absent are called Rh negative (Rh-ve).
- An Rh-ve person, if exposed to Rh+ve blood, will form specific antibodies against the Rh antigens. Therefore, Rh group should also be matched before transfusions.
CIRCULATORY PATHWAYS
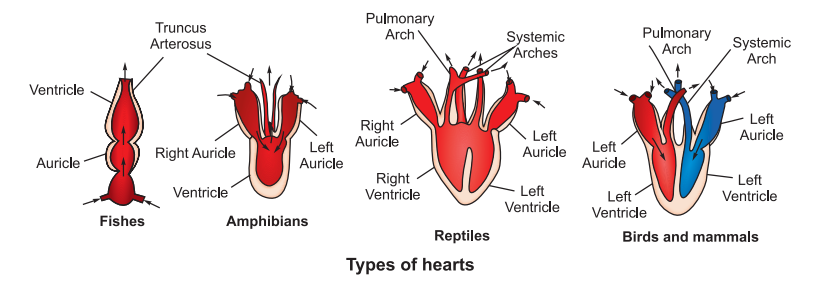
The study of the heart is called cardiology. In invertebrates, evolutionary sequence is absent and most animals possess neurogenic heart.
Vertebrate’s heart shows evolutionary development. They have a single hollow, muscular heart composed of cardiac muscle fibres. These cardiac muscle fibres are responsible for initiating the contractions so the vertebrate heart is myogenic in nature.
Heart acts as a pumping organ of the blood vascular system. It receives blood from and pumps blood to the various organs and tissues of the body. For this purpose, it undergoes spontaneous, rhythmical and ceaseless contractions (beats) throughout the animal’s life.
HUMAN CIRCULATORY SYSTEM
Human circulatory system also known as blood vascular system consist of muscular chambered heart, a network of closed branching blood vessel and the blood.
HUMAN HEART
Internal Structure
The heart is a double pump. It is divided by septa into two halves: the right and the left. Each half consists of two communicating chambers: upper smaller auricle or atrium and lower larger ventricle. Thus, the heart has 4 chambers.
- Auricles: The auricles form a small upper part and act as collecting chambers for the blood returning to the heart. They are demarcated externally from the ventricles by an irregular groove called the coronary sulcus. The two auricles are separated from each other by a partition, the interauricular or interatrial septum. The septum has an oval, thin area called the fossa ovalis. It marks the position of an opening, the foramen ovale, between the two auricles in the foetus. They have thin walls, because they have to force the blood into the ventricles that lie just below them. The posterior wall is smooth; the anterior wall is rough due to the presence of muscular ridges called pectinate muscles, which also extend into the auricle.
- Ventricles: The ventricles act as distributing chambers for the blood reaching from the atria. The two ventricles are demarcated externally from each other by an oblique groove termed the interventricular sulcus: The two ventricles are separated internally from each other by a thick, curved partition, the interventricular septum They have thicker walls than the auricles have, and the wall of the left ventricle is about three times as thick as that of the right ventricle. This is because the left ventricle has to pump the blood to the farthest end of the body, whereas the right ventricle has to send the blood to the lungs, which lie nearby. Correspondingly, the blood entering the aortic arch from the left ventricle is at a much higher blood pressure than the blood entering the pulmonary arch from the right ventricle.
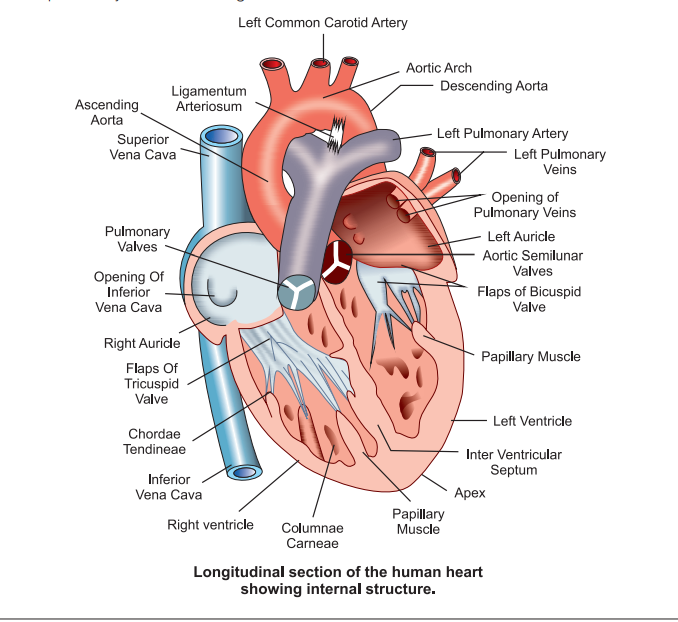
The inner surface of the ventricles is raised into a network of low, muscular ridges called the columnae carneae, or trabeculae carneae, and a few large, conical, muscular elevations termed the musculi papillares, or papillary muscles.
The right auricle opens into the right ventricle through a wide passage, the right auriculoventricular or A-V aperture. This aperture is guarded by a one-way valve called the tricuspid valve. The valve consists of three membranous flaps which are attached to the margin of the right auriculoventricular aperture above but project freely into the ventricle below. Their free lower edges are fixed to the papillary muscles of the right ventricle by a number of tough, cords like structure, the chordae tendineae. The chordae tendineae check the pushing of the flaps into the auricle during the contraction of the ventricle.
The left auricle opens below into the left ventricle by a large passage, the left auriculoventricular or A-V aperture. This aperture is guarded by a one-way valve known as the bicuspid or mitral valve. It consists of two flaps only. The upper edges of these flaps are attached around the left auriculoventricular aperture, while their lower edges project freely into the left ventricle. The free edges of these flaps are connected by chordae tendineae to the papillary muscles of the left ventricle.
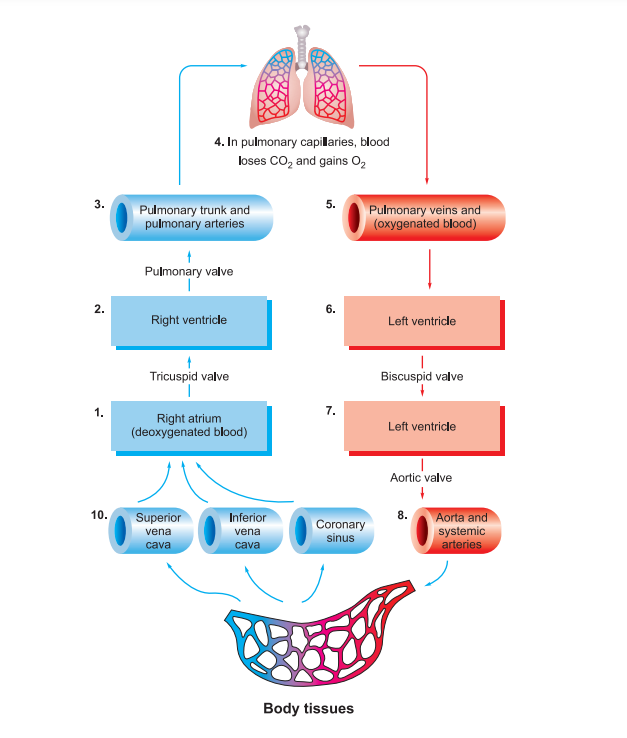
PULMONARY AND SYSTEMIC CIRCULATION
The heart receives blood in the auricles and pumps out blood from the ventricles. From the right ventricle arises a great artery named pulmonary aorta. It divides into two pulmonary arteries, which enter the lungs and break up into capillaries around the lung alveoli. Here, the blood takes up oxygen and becomes oxygenated. Four great veins, called pulmonary veins, two from each lung, return the oxygenated blood from the alveolar capillaries to the left auricle. This course of the blood from the right ventricle to the left auricle of the heart via lungs is called pulmonary circulation.
The left ventricle pumps the oxygenated blood into the great artery termed systemic aorta. It gives off arteries to all the organs of the body except the lungs. These arteries break up into capillaries in their organs. Here the blood becomes deoxygenated by distributing oxygen to the tissue cells. The deoxygenated blood from the visceral capillaries is brought to the right auricle by two great veins known as superior and inferior venae cavae. This course of the blood from the left ventricle to the right auricle of the heart via body tissues (except lungs) is called systemic circulation.
NODAL TISSUES
As we discussed that myogenic heart has inherent and rhythmical electrical activity which is the reason for the heart’s lifelong beat. The source of this electrical activity is a network of specialized cardiac muscle fibers called autorhythmic fibers (auto-self) because they are self-excitable. Autorhythmic fibers repeatedly generate action potentials that trigger heart contractions. They continue to stimulate a heart to beat even after it is removed from the body.
During embryonic development, only about 1% of the cardiac muscle fibers become autorhythmic fibers and are called as nodal tissues. The nodal tissue consists of (a) Sinuauricular node (S-A node), (b) Auriculoventricular node (A-V node), (c) bundle of His or auriculoventricular bundle (A-V bundle), right and left bundle branches, and (d) Purkinje fibres.
- The S-A node is located in the wall of the right auricle slightly below the opening of the superior vena cava. This is the place where the sinus venosus is incorporated in the embryo.
- The A-V node lies in lower left corner of the right atrium close to the atrio-ventricular septum.
- The bundle of His originates from the A- V node, passes downward through the inter interventricular septa, and divides into the right and left bundle branches, one going into the wall of each ventricle.
- In the walls of the ventricles, the two branches break up into a large number of Purkinje fibres that are distributed to the entire musculature of the ventricles.
CARDIAC CYCLE
The heart pumps the blood to all the parts of the body. It pumps out over 7,000 litres of blood daily. Force that propels the blood comes from the contraction of cardiac muscle, which contract due to the cardiac impulses settled by the nodal tissues. To pump out blood, the heart chambers undergo alternate contraction called systole and relaxation termed diastole. The contraction of a chamber decreases its volume and forces the blood out of it, whereas its relaxation brings it back to its original size to receive more blood.
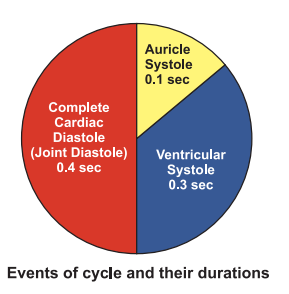
One complete heartbeat (cardiac cycle) lasts for about 0.8 seconds which occur in regular sequence of three events:
- Joint diastole, or complete cardiac diastole (relaxation of both auricles and ventricles)
- Ventricular systole, and
- Auricular systole
These events are repeated in a cyclic manner during each heartbeat, and make the blood flow through the heart chambers in a specific manner and direction.
Cardiac Output The volume of blood pumped by the left ventricle into the systemic circuit per minute is called heart output or cardiac output. It depends on two factors: heart rate (pulse) and stroke volume (the amount of blood pumped by the left ventricle each time it contracts) Heart beats 72 times per minute, and pumps out about 70ml. of blood during each beat.
Thus, 72 × 70 or 5040 ml (roughly litres) is the heart or cardiac output. This is only a little less than the total amount of blood (about 6-8 litres) present in the body.
Heart Sounds
- First Heart Sound: It is low-pitched, not very loud and of long duration. It is produced by the simultaneous tight closure of the tricuspid and bicuspid valves at the start of ventricular contraction.
- Second Heart Sound: It is higher pitched, louder, sharper and of short duration. It is produced by the closure of the semi-lunar valves at the start of ventricular relaxation. It lasts for 0.1 seconds. Both the heart sounds can be heard by placing ear or better stethoscope receiver on the left side of the chest wall.
ELECTROCARDIOGRAM (ECG)
A permanent record of the electric events occurring during a cardiac cycle made on a graph paper in a waveform is called electrocardiogram. The electric events include depolarization and repolarization of the auricles and ventricles bringing about their contraction and relaxation. The instrument used for recording the heart’s electric events is named electrocardiograph. The electric current produced by the heart is picked up by the surface electrodes placed in various positions on the body (two arms, left leg and chest) and passed through a string galvanometer present in the electrocardiograph.
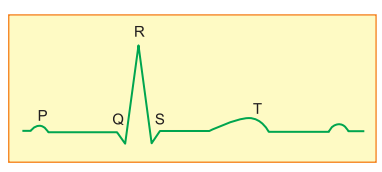
A typical human electrocardiogram shows five waves or deflections, which are conventionally called P, Q, R, S and T. The Q, R, and S waves are sharp whereas P and T waves are blunt. The part of the base line between any two deflections is called interval.
The P-wave represents the electrical excitation in the fibres of S–A node causing depolarization of the atria, which leads to the contraction of both the atria. The interval PQ represents contraction of the auricles. This takes 0.1 second. The QRS complex represents combined depolarization of A – V node and bundle of His and repolarization of S – A node. The RS of QRS complex and ST interval show contraction of ventricles. The T wave indicates the repolarization during ventricular relaxation. The end of the T-wave marks the end of systole.
Obviously, by counting the number of QRS complexes that occur in a given time period, one can determine the heart beat rate of an individual. Since the ECGs obtained from different individuals have roughly the same shape for a given lead configuration, any deviation from this shape indicates a possible abnormality or disease. Hence, it is of a great clinical significance.
PORTAL CIRCULATION
- Portal Vein: A vein which collects blood from one organ by one set of capillaries and distributes blood to some other organ by another set of capillaries instead of sending it to the heart is called a portal vein.
- Portal System: A portal vein together with the small veins by which it receives blood and the capillaries by which it supplies blood to a specific organ forms a portal- system. A portal system is named after the organ to which it carries blood. The vertebrates have 2 or 3 portal systems –hepatic, renal and hypophysial.
- Hepatic portal system: It is present in all vertebrates including man.
It carries the venous blood from the alimentary canal, pancreas and spleen to the liver, hence its name.
Components: The hepatic portal system includes a single large vein, the hepatic portal vein. This vein receives a number of small veins from the different regions of the digestive tract and its associated structures. At its other end, it bifurcates into right and left branches, which enter the corresponding liver lobes and break up into capillaries to supply the blood. Blood from the liver is carried by a pair of hepatic veins to the inferior vena cava.
- Renal portal system: It is present in fishes and amphibians, is reduced in reptiles and birds, and is absent in mammals. It supplies the blood from the posterior region of the body to the kidneys by way of renal portal veins, hence its name. It enables the kidneys to remove waste products from the blood before sending it to the heart via renal veins and postcaval. Gradual reduction of the renal portal system in reptiles and birds and its disappearance in mammals is an evolutionary change in which the blood from the posterior region of the body is progressively carried directly to the postcaval.
- Hypophyseal portal system: It is a minor portal system in the pituitary body. A hypophyseal portal vein connects blood from the hypothalamus of the brain and distributes it to the anterior lobe of the pituitary body. This portal system enables the hormones from the hypothalamus to reach the anterior pituitary lobe.
Portal circulation: The flow of blood through the portal veins to certain specific organs other than the heart is called portal circulation.
BLOOD PRESSURE
Blood pressure is the pressure against the walls of the blood vessels produced by the discharge of blood into them by contractions of the left ventricle. It is measured as millimeters of mercury by the instrument called sphygmomanometer. It has a high systolic value (normal 120 mm Hg) and low dialostic value (normal 80 mm Hg). The difference between the two is called pulse pressure.
Hypertension: It is sustained rise in arterial blood pressure or high blood pressure with systolic more than 140 mm Hg and diastolic more than 90 mm Hg. The reason is stiffening of arterial walls due to ageing, thickening of arterial walls due to cholesterol deposition, chronic vasoconstriction of arterial walls, varicose veins, obesity, toxins, hormones, defective kidneys, etc. Hypertension caused by hormones (e.g. epinephrine, aldosterone, renin) is called secondary hypertension. Other forms of hypertension are known as primary or essential hypertension. The latter account for 90% of the cases. High blood pressure harms three vital organs – heart, brain and kidneys. It makes heart to overwork due to which congestive heart disease develops quite early. A blood pressure of 220/120 mm. Hg may cause internal haemorrhage due to rupturing of some blood vessel. Cerebral haemorrhage causes stroke or CVA. Damage to optic arteries leads to blindness while a similar damage to renal vessels causes nephritis. It leads to renal failure.
Hypotension: Fall in the arterial blood pressure is called low blood pressure or hypotension. (Systolic below 110 mm Hg and diastolic below 70 mm Hg). It is caused by low metabolic rate, starvation, anemia, chronic, vasodilatation of arterioles, lower pumping activity, valvular defects, nervous disorders Addison’s disease. It may cause fainting.
REGULATION OF CARDIAC ACTIVITY
Heart is myogenic in nature which means it has the tendency to contract on its own. The rate of the heartbeat is, however, controlled by the nervous and endocrine systems.
(a) Nervous Regulation: The cardiac centre lies in the medulla oblongata of the brain. The cardiac centre is formed of cardio-inhibitor and cardio-accelerator parts. The former decreases the rate of heart beat and the latter accelerates it.
The cardio-inhibitor is connected with the heart through vagus nerve (it carries– parasympathetic nerve fibres) and cardio accelerator through sympathetic nerve fibres.
Sensory fibres extend from the receptors present in the superior vena cava, aorta and carotid sinuses to the cardiovascular centre of in the medulla oblongata.
The impulses received from the aorta and carotid sinuses decrease the heart rate, whereas the impulses from the vena cava increase the heart rate.
(b) Hormonal Control. Adrenaline (epinephrine) and noradrenaline (norepinephrine) hormones are secreted by the medulla of the adrenal glands. Noradrenaline accelerates the heart beat under normal conditions while adrenaline does this function at the time of emergency. These hormones directly influence the SA node.
Blood pressure can also be controlled by the heart by secreting ANF (Atrio- natriuretic factor) which helps in decreasing the blood pressure.